.svg)
.svg)
.svg)
How patient access teams can use AI to save time, improve accuracy, and reduce denials
AI helps patient access teams work faster, cut errors, and reduce denials—without replacing human judgment. By handling repetitive tasks like record review, letter drafting, and payer follow-ups in a HIPAA-compliant setup, AI boosts capacity and improves quality so more patients get care on time.

Introduction: AI is here to support humans, not replace them
Our philosophy on current capabilities of AI can be summed up in one sentence: “We love AI, but we should all be AI skeptics.”
We believe AI won’t fully replace humans in patient access anytime soon, and for good reason. Reimbursement is a minefield, defined by complex workflows, strict compliance requirements, and a variety of edge cases that defy simple automation. But while full replacement is unlikely, the opportunity to augment and accelerate human work with AI is both real and powerful. Done right, AI can help teams navigate complexity more efficiently, freeing up capacity to focus on other, more strategic tasks. AI can also help in getting cases approved in otherwise unfeasible situations (due to time that would’ve been required for a human to manually review everything). Ultimately, all of this leads to better outcomes for patients.
Like a front-line employee, AI is good at implementing detailed instructions and can even “reason” on those instructions. However, it does not have the context to fully replace human judgment. Humans still need to give instructions and evaluate outputs, making corrections where needed. In other words, AI follows the playbook, but humans write it and call the fouls.
AI drives operational efficiency by handling repetitive administrative work, freeing people’s time and cognitive capacity for higher‑value decisions. One of AI’s greatest strengths is that it is indefatigable: where humans tire after hours of concentrated work and start producing lower-quality outputs, AI remains consistent.
Top five AI applications for patient access teams
This section details various ways in which AI is being used in patient access.
1. Comparing the patient’s case against payer criteria and clinical guidelines
In a perfect world, for any one patient case, a human tracks down the specific, most-recently updated payer policy for a given treatment, tied to the patient’s plan, and carefully reviews the patient’s medical records to assess whether all policy criteria are met.
In reality, though, this level of diligence is uncommon, not because it lacks value, but because it’s simply too time-consuming. Documentation overload and policy variability make it nearly impossible to apply this level of scrutiny consistently using only human effort. Depending on the complexity of the intervention and the patient’s medical history, this process might take hours or even days per case.
Enter AI: AI tools can automate reviewing hundreds of pages of medical records, quickly locate the appropriate payer policy, and compare against payer criteria and clinical guidelines. Then the human can “check the AI’s work.” As an example, below are two screenshots from our software.
FIGURE 1: AI Summary
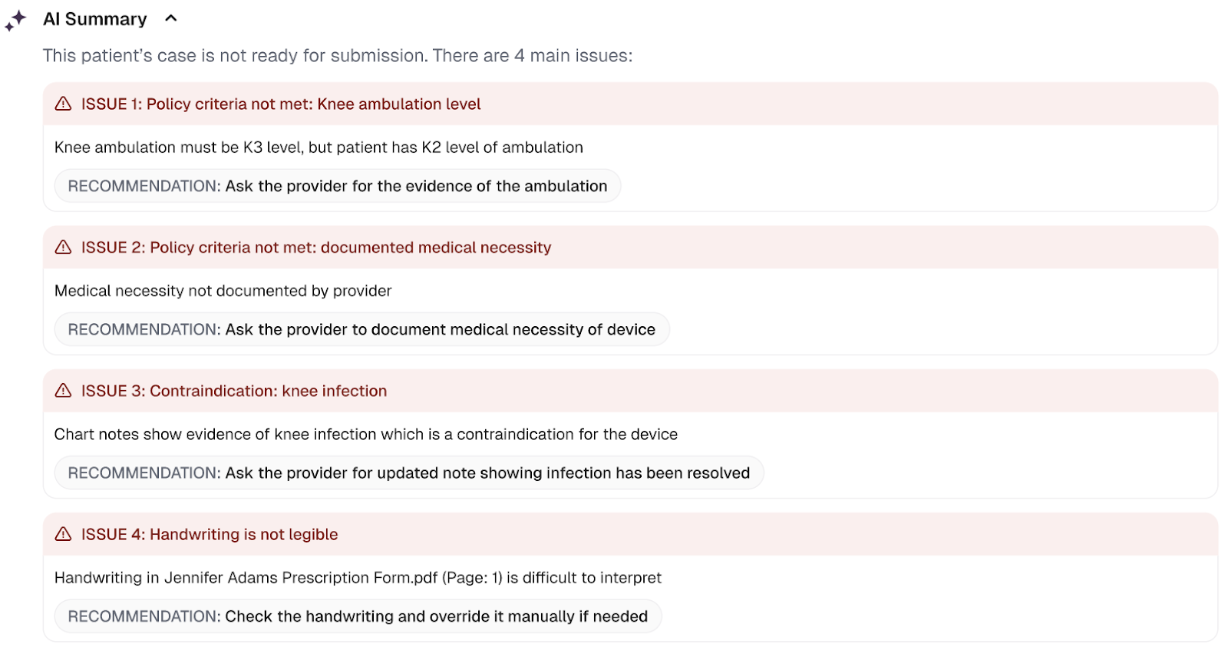
In “ISSUE 1” above, the AI flags an approval risk by surfacing documentation indicating that the patient has an ambulation level of K2; however, the clinical policy for the relevant insurer requires that the patient ambulate at the K2 level.
AI can review the patient file line-for-line against the exact payer policy and clinical guidelines in minutes, and it can flag missing information (the red “ISSUES” shown above) to prevent sending an incomplete submission. Suppose a policy doesn’t exist yet for a product still working on broader payer coverage. In that case, the AI can still generate a robust justification based on available clinical evidence and guidelines (e.g., specialist society recommendations), just as a human patient access professional would.
FIGURE 2: Citations for all AI-extracted data with source documents in side-pane
.png)
Human reviewers should be able to verify any of the extracted data from the case against the source documents to ensure the correctness of the output.
We strongly recommend that a qualified human review AI‑generated outputs for accuracy, especially during the initial rollout of an AI reimbursement tool. As shown in FIGURE 2, our tool lists the extracted data (in this case, the patient’s past treatments, a common health insurance requirement for illustrating the patient has attempted many other treatments before needing to resort to a typically more expensive or innovative treatment) and attaches a source citation to each item, which reviewers can click into and quickly verify the data against the correct clinical documents in a side-pane.
When the evidence is unclear or complex, AI can review far more information – clinical documents, studies, case reports – than a human reviewer realistically has time to process. It can quickly scan the literature to surface subgroups or outcome signals, suggesting a patient could benefit from a certain treatment. By contrast, humans typically get only as far as payer criteria or broad guidelines due to the time involved with a more robust review.
In plain English: AI does the heavy lifting by finding relevant evidence quickly, but humans stay in the loop to confirm accuracy and make the final call, especially when the stakes are high or the case is complex.
2. Generating customized patient case documents for submission
Many patient access teams still rely on stock templates when completing insurance paperwork. They scroll through the patient’s chart (looking for name, date of birth, provider NPI, etc.) one line at a time. Each field is quick on its own, but the minutes add up, especially for the longer sections like patient history or the detailed explanation of why they meet the insurer’s criteria.
Templates work in a pinch, but they’re far from ideal; they’re used only because there isn’t enough time to craft a custom letter for every single case. And insurers have been known to catch on to templates and deny cases as a result. An AI system, however, can gather the right details and generate a personalized document in seconds. While there are many software offerings to auto-insert fields into templates, generative AI now allows for more customization.
FIGURE 3: Example AI-Generated Prior Authorization Cover Letter
.png)
AI can now generate fully tailored prior‑authorizations, appeals, and other justification letters (all in the payer’s own language) and tie every sentence back to the exact policy line or guideline it fulfills.
Because it works at machine speed, an AI system can also pack in far more nuance than a busy human ever could. Think of those complex cases where you’d love to show why the patient has already failed every alternative therapy the insurer might suggest, or demonstrate how the patient isn’t a fit for the preferred treatment due to contraindications or comorbidities buried in their clinical history, or even highlight how they happen to match the most responsive subgroup in a clinical trial. AI can identify and integrate those details automatically.
That way, your team gets depth, accuracy, and a document that’s ready to win approval without the extra hours.
3. Submitting documents to payers
In some cases, AI can handle the submissions of these documents, but current tech solutions for automated submissions are underdeveloped. Automation is certainly possible for some payers, but not all. This is changing over time, as more payers adopt standardized electronic means of submission.
Today, a patient‑access specialist has to submit the prior auth or appeal (sometimes by fax or mail…or even mail!), then chase the case online. As automation increases, AI agents (who can conduct tasks on a computer just like a human would) can become conduits for submissions, both in payer portals and via API (i.e. electronically in the backend). While manual submissions are still often quite necessary today, we expect this to change in the future.
4. Phone calls with payers
Talking to payers is still painfully manual. A patient‑access specialist often has to spend ages on the phone for status updates.
Voice AI, however, enables the AI to speak to a payer rep just like a human, which includes navigating phone trees, waiting on hold, and actually discussing relevant case information. This is particularly useful for common, simple calls such as following up on a submission to ensure it’s being processed by the payer. Paxos now has this capability. And over time, more advanced calls, like escalating a request for a courtesy review, should become possible as well. Of course, as with any other application of AI, there should be a human “fallback” to do a pulse check or tweak the script where necessary.
Could payers forbid AI callers? Maybe, but they’re rolling out their own bots, so the future probably looks like AI talking to AI. Even in the short run, an assistant that waits on hold for you frees staff to focus on higher‑value work instead of listening to hold music.
5. Generating an audit trail
Industry research indicates audits (whether from payers or regulators) are becoming more frequent and more thorough. Right now, teams scramble to pull paperwork, slowing down every case and throwing workflows off track. AI can play a big role here: It runs “mock audits” upfront, checking the patient file against every policy, flagging gaps, and logging a clean, traceable record as it goes. All that data lands in an audit‑ready dashboard. When the real audit notice arrives, you export the file and hit send – no fire drill required.
FIGURE 4: Example of an AI-Generated Audit Report for a Mock Case
.png)
Aggregating data in such a clean and digestible format could also expose other meaningful insights (unrelated to audits), such as trends on various clinical policy criteria for your product (e.g. are payers focusing on certain criteria across the board or writing very diverse coverage policies?).
AI can also enforce privacy policies in real time, blocking sensitive outbound text, flagging odd access patterns, and logging every prompt and redaction for instant audit readiness. That level of compliance would be much harder to achieve with human guardrails.
In compliance-heavy areas, having the right software in place doesn’t just improve efficiency; it also ensures full traceability. Every step, decision, and document is logged and accessible, creating a clear audit trail that’s critical for meeting regulatory requirements and reducing risk.
Addressing Privacy Concerns
Contrary to popular belief, AI doesn’t have to be a privacy risk; in fact, it can raise the compliance bar. Leading platforms like OpenAI, Anthropic, and AWS now sign HIPAA Business Associate Agreements (BAAs), so you can run models inside HIPAA‑eligible clouds with built‑in encryption, network isolation, and audit logging. They can easily be configured so the AI labs delete your data and avoid training AI models on it.
Note: The chatbot interfaces for most large language models (LLMs) are not HIPAA-compliant by default, so you should not input any protected health information (PHI) into them. To use LLMs in a HIPAA-compliant way, you must sign a Business Associate Agreement (BAA) with the vendor and access the model via secure, API-based infrastructure designed for handling PHI.
AI is already being applied in many compliance-heavy industries (including healthcare) because teams can choose the security dial‑setting that fits their risk profile, from turnkey BAA‑backed clouds, to virtual private clouds, all the way to fully self‑hosted models behind your own firewall while the AI works as a compliance co‑pilot.
Conclusions and practical advice for you and your team
AI in patient access is about amplifying human effort, not replacing it. Though we’ve listed a few great potential applications of AI tools like Paxos, we recommend you start small. Pick one high‑friction step (e.g. case assessment compared to insurance policy, letter drafting, etc.) and let AI do the first pass while your team reviews. Track time saved and case outcomes, then expand the rollout.
Done right, AI can increase the capacity of patient access teams, improve the quality of submissions through cross-referencing criteria for each patient, and ultimately get more patients access to the care they need.
For more information, book a demo here: Paxos Health.

.svg)