.svg)
.svg)
Patient Access, Powered by AI
Empowering patient access teams in medtech, DME, and beyond to 3x their productivity and increase approval rates. Our tool can be used by patient access teams, providers, or patients.
We customize our AI to your specific workflow.
Experience With All Major US Payers





.svg)





.svg)





.svg)





.svg)
































How We Help
We focus on complex reimbursement workflows, such as when the documentation burden is high, there are negative or silent payer policies, a product is new-to-market, etc.
Beyond basic form-filling, our AI distills exhaustive patient data into robust arguments that resonate with payers, even when no positive policy exists.
This means increased provider and patient confidence in reimbursement.
Case Studies
.svg)

With a CPT Category III code and an anticipated transition to a permanent Category I code in 2026, we built this company's reimbursement and patient access infrastructure from the ground up.
.png)
Streamlining payer approvals for Sleep Apnea Surgery Center's EASE procedure, an innovative minimally invasive procedure that payers frequently denied as "experimental." Paxos developed a comprehensive patient advocacy program with customized appeals and network gap solutions to secure coverage approvals and reduce administrative burden on the practice.
We support many major CRMs


%20(1).png)
%20(1).avif)
%20(1).png)
.png)


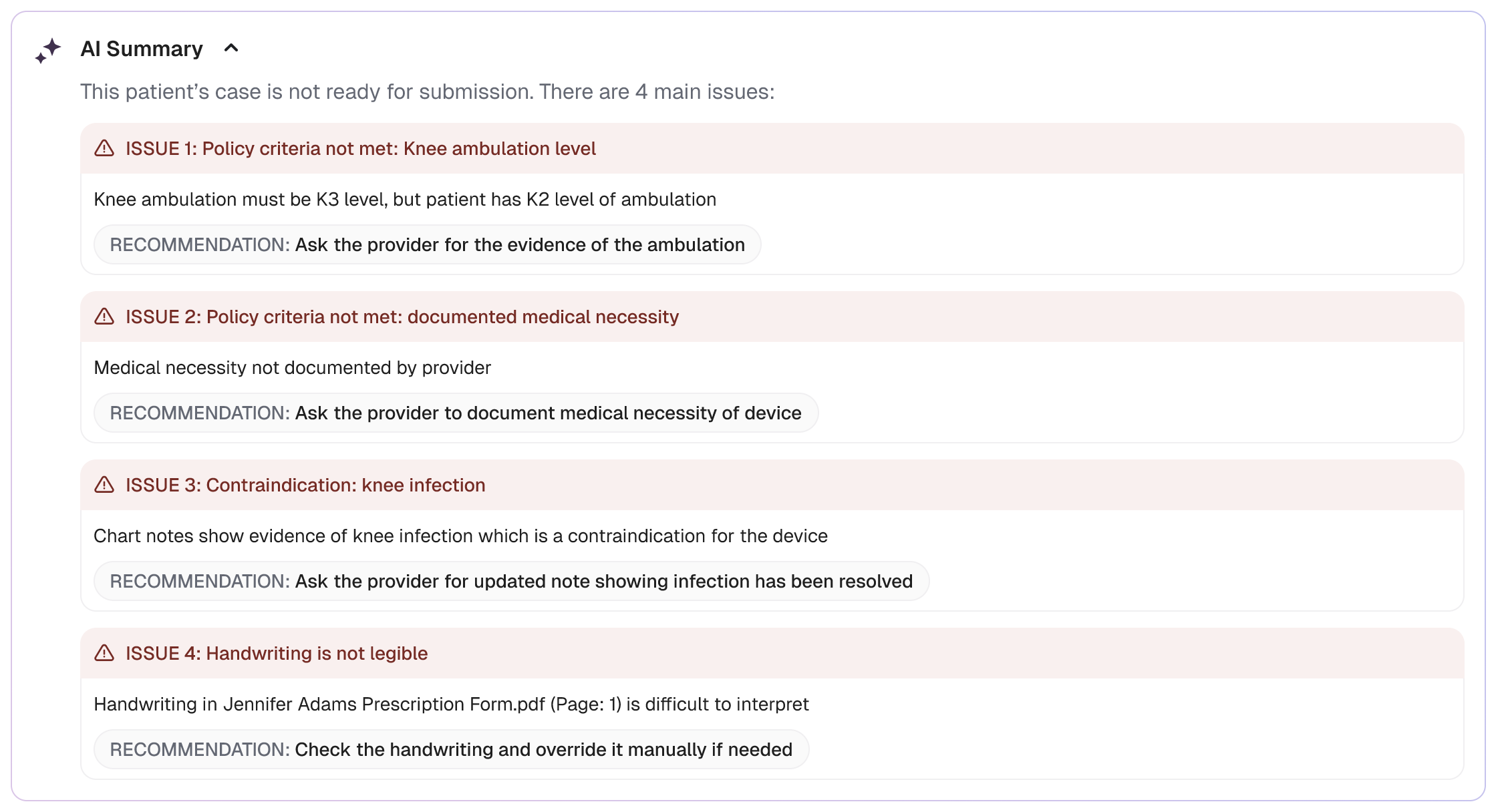
See Our Product
Want to improve your company’s reimbursement processes? Book a demo today.
.svg)
* Refers to values extracted from source documentation. Based on internal testing comparing to human ground truth. Further information available upon request.





.svg)






.png)
.jpg)
%201.png)
.png)
.avif)
